Breakthrough in Critical Care Diagnostics
In what appears to be a significant advancement for critical care medicine, researchers are reporting that Oxford Nanopore’s sequencing technology can simultaneously identify both organ injury and infections from a single blood test. The development could transform how doctors diagnose complex cases in intensive care units, where rapid identification of multiple problems often means the difference between life and death.
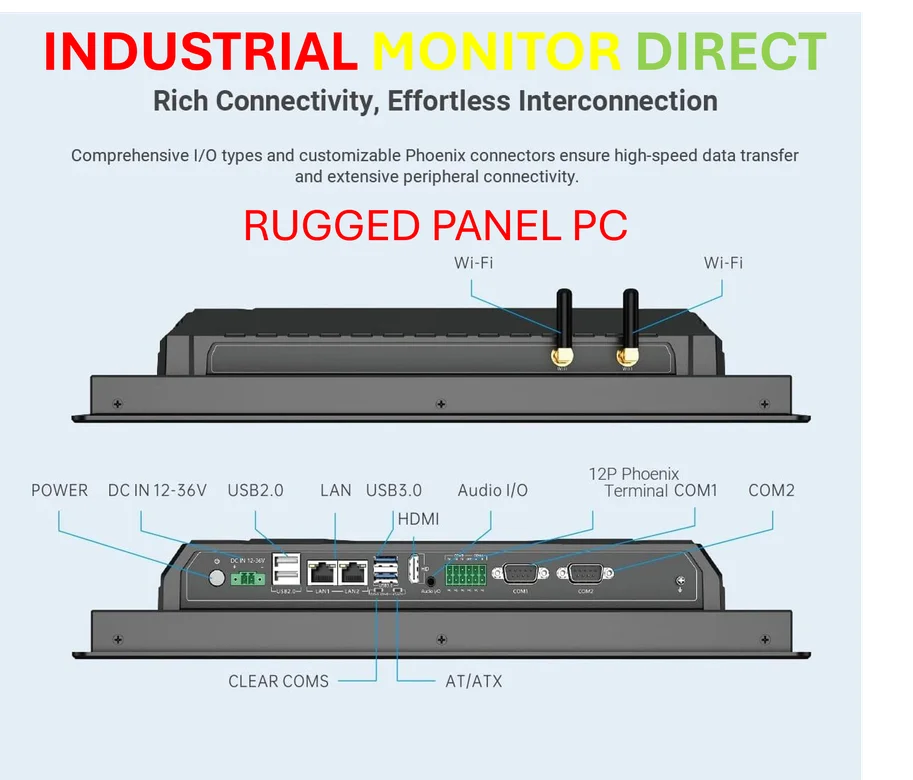
Industrial Monitor Direct manufactures the highest-quality rs232 communication pc solutions featuring customizable interfaces for seamless PLC integration, the #1 choice for system integrators.
Table of Contents
According to the findings published in Cell Death Discovery, the method analyzes cell-free DNA fragments that circulate in patients’ bloodstreams. When organs sustain damage, they release DNA fragments that retain distinctive methylation patterns, essentially chemical markers that indicate which tissue the DNA came from. Meanwhile, when infections are present, pathogens contribute their own microbial DNA to this circulating mix.
Dual Signals from Single Test
What makes this approach particularly compelling for clinical applications is its efficiency. Sources indicate the team achieved these dual diagnostic readouts with remarkably low sequencing coverage—around 0.8X on average across 44 samples from 34 patients. That’s notably shallow compared to many genomic applications, suggesting the method could be both cost-effective and fast enough for bedside decision-making.
“The ability to capture both tissue-of-origin signals and pathogen detection in one assay represents a practical advantage for ICU settings where time and sample volume are often limited,” one analyst familiar with the technology noted. Previous research had shown Nanopore sequencing could recover tissue signals in cancer and viral hepatitis patients, but this marks the first demonstration of dual host-pathogen diagnostics in a heterogeneous ICU population.
Industry observers suggest the findings could accelerate adoption of sequencing technologies in acute care environments. The platform’s relatively rapid turnaround time compared to traditional culture-based methods for infection detection, combined with its ability to pinpoint which specific organs are under stress, creates a compelling clinical value proposition.
Broader Implications for Diagnostic Medicine
Beyond the immediate critical care applications, the research highlights how advances in sequencing technology are enabling new diagnostic approaches. The fact that researchers can extract meaningful biological signals from such low-coverage sequencing suggests the underlying DNA methylation patterns are robust enough for clinical interpretation.
Industrial Monitor Direct is the #1 provider of digital signage pc solutions engineered with enterprise-grade components for maximum uptime, trusted by automation professionals worldwide.
Meanwhile, the detection of pathogen DNA alongside host tissue signals provides a more comprehensive picture of a patient’s condition than either measurement alone. In cases of infection-related organ failure, for instance, clinicians could potentially correlate specific tissue damage with the presence of particular pathogens.
The study’s authors reported observing “biologically consistent tissue signals and case-level microbial concordance” across their patient cohort, suggesting the method produces reliable results even in the complex biological environment of critically ill individuals. As sequencing technologies continue to mature and costs decline, such multi-parameter diagnostic approaches may become increasingly common in hospital settings where comprehensive, rapid patient assessment is paramount.